As I’m currently bed-bound, I thought I’d try and get my brain back into some kind of ‘gear’ and write an update on my miscarriage journey. The final one, I hope.
See also:
READ MORE >> Miscarriage & Me.
READ MORE >> Miscarriage & Me // An Update.
READ MORE >> Miscarriage & Me // An Update: 2.
—–
After lack of bleeding from my Medical Management, we went into the scan on Monday 2nd October kind-of hopeful. We had the Consultant Obstetrician and Gynaecologist, Dr Anita-Rao, along with our Sonography staff. Dr Anita-Rao had all my (many) previous scans in front of her, I knew by the movements of the scanner and her face that it wasn’t good news…
She put the probe down and moved the screen towards us. The sodding sac was STILL there. But it gets worse… not only was it STILL there, but it had GROWN. The empty sac had increased. I couldn’t believe it. I’d lost so much tissue and blood during my Medical Management, so how could this have happened? It was all kinds of insane. I went into that bubble of your own, where you can hear the sounds of conversation – but can’t make out the words. According to James, the Consultant explained that the hormones given during the Medical Management had encouraged an increase in amniotic fluid – thus enabling the sac to grow/fill with fluid. She showed us a heat map, indicating no blood flow, no heart beat, no life. By this point I would have been 16 weeks pregnant – the sac had increased in size from 7 weeks and 1 day (at the 12 week scan) to measuring 8 weeks. Dr Anita-Rao advised the only way to go forward with this now was Surgery. The dreaded (ERPC or ERPoC, which stands for Evacuation of Retained Products of Conception. You might hear it called it a D & C too) which is under anaesthetic.
Dr Anita-Rao then said “Ok Claire, let’s get you sat next door and make you a bit more comfortable”. To which I jumped off the bed and shouted “WHAAAAAAAT!”. As I was in my little bubble, I didn’t catch what the conversation actually was, and I thought they were going to take me off to theatre, there and then. Obviously, my first thoughts were – “My darling Eli! – he’s at school – I need to see him”.
What they actually meant was, they wanted to go back to the Quiet Room to discuss the procedure/dates/times.
Midwife Amelia came back to us, once again – so wonderfully compassionate and with genuine empathy. We discussed the Surgical Management of Miscarriage and she handed me the instructions for patients ahead of General Anaesthetic. I was booked in for the morning surgery on Wednesday 4th October – therefore, had to be at Broomfield Hospital for 7:30am (being Nil By Mouth from 2:30am).
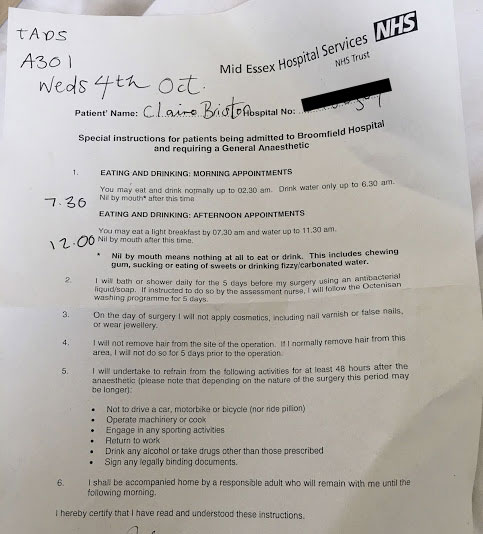
LOOK AT THIS LIST.
JUST LOOK.
My favourite thing on this list? The SILVER LINING in this whole experience…. take a look at number 5:
5) I will undertake to refrain from the following activities for at least 48 hours after the anaesthetic (please note that depending on the nature of the surgery this period may be longer);
- Not to drive a car, motorbike or bicycle
- Operate machinery or cook
- Engage in any sporting activities
- Return to work
- Drink alcohol or take drugs, other than those prescribed
- Sign any legally binding documents
YAAAAAAS to no driving, cooking (and cleaning) or signing of legal documents. Though, this did implicate James working – thankfully he works for a very understanding company. We don’t have any family down here, so we’re reliant upon eachother in times of need – and our friends help out around us as best as we can all manage.

So that was that. We had all our questions and concerns answered by Midwife Amelia and given well wishes for the future. I also had to not apply any perfumes and wash with this ^ Octenisan – in aid of protecting against MRSA.
Wednesday 4th October
A301 – Theatre & Day Surgery – Broomfield Hospital
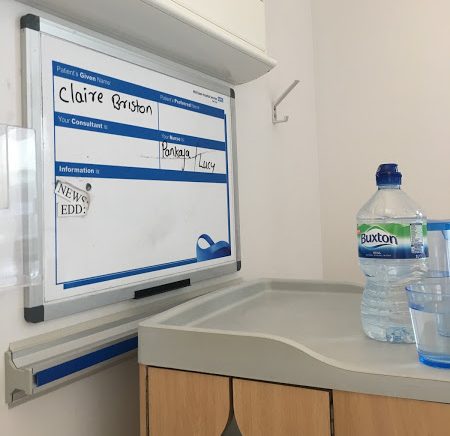
Upon arrival at 7:30am, we were in a large waiting area of A301. My name, along with around 30 other names, was called and we were escorted by the Pre-Anaesthetic team to ‘Recovery 2’ ward, waiting area. There were separate waiting area’s for Males & Females (adult surgery, only), the signs said this was in line with ‘protecting dignity’.

We were both acknowledged as being there – despite me being the patient. Which I thought was really kind of the staff. We both sat on a green chair each – all freshly cleaned (with green warning stickers to say so). I reclined the chair and waited for my first set of assessments.

We weren’t waiting long before I was ushered off to a side cubical and given details of who I would speak to and having my ob’s taken. After a bit of back and forth between waiting areas (and a lot of apologies and friendly chatter), I was sat down finally in another cubicle and awaited a chat with my Anaesthetist. Dr John finally came along – he had a familiar face – a bit like that of Actor James Redmond. I talked through how petrified I was of ‘being put to sleep’. He talked through the process, reassured me no-end and I felt so much better about the entire situation. I signed some forms and he said he’d see me again, just before theatre.
I then awaited a chat with my surgeon, Dr Mistry. Dr Mistry, again settled my nerves about the actual procedure. We talked about the fact I was left in quite a state after an Episiotomy gone very wrong, following the birth of Eli (which left me with early-caught-Sepsis and a very damaged undercarriage that was left to heal ‘on it’s own’ for neigh on 2 years). (Yep, not had a lot of luck on my side to be honest!)



I was then told that I was at the bottom of the list for the morning surgery. My last meal was at 9pm the night before (having only had a bit of water when I got up at 5:30am). By this time it was 10:30am and I was SO THIRSTY! I drink a lot of water, every day – more out of habit than anything else! But it was driving me crazy not being able to even wet my mouth.
I was given lots of updates and eventually told at 11:45am that I was ‘next’.
12:15 arrived and a lovely lady came with all my notes to take me to theatre. James and I said our “I love you’s” and off I went. I know it was a straight forward procedure, I know it wasn’t complicated, but the fact I was being put under anaesthetic, as a MOTHER, petrified me. You just don’t know how your body will react to things like anaesthesia. What if I didn’t wake up again? That was my big fear. Not the pain or discomfort. The FEAR of being put to sleep.
I thought I’d be taken down to the theatre on a bed, but instead, I had to walk there. It was a short walk. But I balled my eyes out the entire way. The nurse who took me along was brilliant – she wrapped her arms around me tightly and told me that she knew it was scary, but it would be fine. I needed her comfort. We walked into a room marked, Theatre 18. Once inside, she explained that this was the Pre-Anaesthetic room, where I would be put to sleep – once under, I’d then be taken through to the actual theatre. She took off my sliders and undid the back of my hospital gown and helped me up onto the surgical bed.
She stayed with me for a little while – then the Anaesthetic room began filling with medical staff. I looked around at the mass of machines and equipment. I could see the theatre ahead of me, through some double doors. A few members of the surgical team went through the doors – the light above now highlighted ‘IN USE’. I closed my eyes each time someone went through the doors. I didn’t want to ‘go to sleep’ to the view of the theatre. It was insanely bright and white. And frankly, it scared me. Maybe I’ve seen too many hospital programmes!
My lovely nurse then said her goodbye’s and passed me over to Julia. Who prepped me with chest electrodes, a blood pressure band & finger monitor and tucked me up under a blanket. She gave me tissues and stroked my hair. I was trying my hardest to be strong. But my god, it’s so hard when people are just so bloody lovely and all you’re talking about is your wonderful family.
Dr John prepped my arm for the cannula, as we talked about our trips to Cornwall. Everyone chirping in about their own experiences – so laid back! There were around 6-8 staff in this tiny, dim-lit surgical room by this point. My surgeon arrived with another doctor. All smiles.

Dr John administered the cannula (OUCH) to my left arm; and washed my vein out with saline. I remembered that cold feeling running down my arm, from when I had the drip during labour with Eli. The chatter was constant – this time turning to accents and how we’d managed to ‘end up’ in Essex. I could feel another fluid going down my arm and began fighting to keep my eyes open – focussing my attention on that ‘IN USE’ sign above the theatre doors – for I knew when that was out of focus, I’d be gone. I asked “have you given any anaesthetic yet, because I feel a bit weird?”. I then remember thinking, ‘they’re all chatting away to me so they can tell when I’m asleep – so I’m going to keep on chatting, so they can’t trick me’. It must have been Pre-Surgery logic… or something.
The last words I heard were “It’s now going to feel like I’ve just given you a few large Gin & Tonic’s, ok?”. I remember nodding and feeling really cosy… and that was it. Out like a light.
Fast forward to 1:30pm and I was on the first Recovery ward. My waking words were repeatedly “I love the NHS” and “Save the NHS” and “compliments to the staff”. YAAAAAAAS to #SAVETHENHS. The nurse who was looking after me told me to stop being apologetic (!!!) and that I was fine and everything went as it should have. She then asked for my consent to check the pad that I’d woken up with. I was bleeding a normal amount – phew. She then told me it had taken a little while for me to come round. I was surprised, shocked… and then felt so incredibly sick. She grabbed one of those egg-cup dishes and kept checking my blood pressure. It was slightly high. My temp was 37.8. I felt so, so sick and dizzy. But just so relieved to be awake! She said they’d already given me painkillers and anti-sickness medication – then she administered a little more anti-sickness medication for me. I then began feeling a lot better. Soon after, my stat’s began to normalise. In the time that I was settling down, I saw 3 patients transferred to the recovery ward post-surgery. It was so interesting to see. The quality of care was just incredible. The teamwork, the processes and attention to detail was above and beyond.
By 2:30 my nurse was happy to have me transferred back to the Pre-Anaesthetic ward, where James would be called to come and find me – I can’t remember her name, sadly. I wish I could. I was wheeled back to the ward in my post-surgery bed, feeling ridiculously happy? Not sure if this was a side-effect of the anaesthetic or if it was pure relief and the joy of feeling proud of oneself.

I played an ill-timed joke on James before he arrived on the ward – of which, he’s still pretty annoyed with me about – so I won’t go into it. Hah. But here I am, about 90 mins post-surgery. I had to be linked up to oxygen for a little while after as my level’s hadn’t settled.
But man-oh-man, that first water since 5am was SO GOOD. I drank a litre in a matter of minutes. It must have been about 3/3:30 by this time and I was told I could eat! SO EXCITED. I had a cup of tea and toast on their way. I don’t think ANYTHING will ever beat that tea & toast you have after childbirth – but this one, was pretty damn close!

James spread the butter and marmite while I supped on that lovely, perfect, cuppa! Oh it was so good. I had little pain/cramping. Nothing major – and like I say, I felt pretty bright in myself. I just couldn’t wait to get home to my boy.
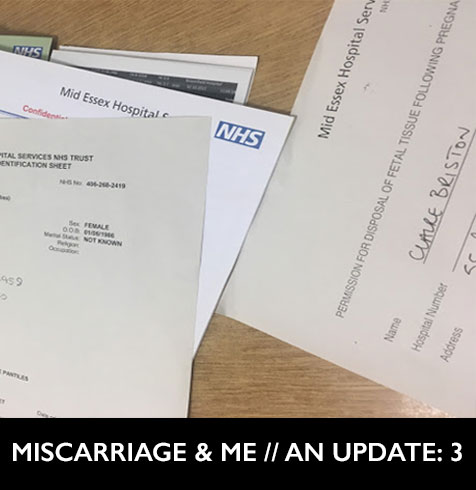
I had a few after-care instructions to go over with the Senior Staff Nurse on the ward and would then be discharged. I signed a form to allow the Pregnancy Products to be disposed of, after investigation. I was given all the warning signs and symptom’s to look out for post-surgery – and told to expect bleeding for around 7-10 days.
Now then – I got home expecting to be filling pad’s and pad’s with blood. But again – I’ve had nothing. No idea if this is good or bad – but Dr Google tells me that this can be pretty normal. Infact, bleeding can sometimes begin a few days post-surgery, resulting in heavy bleeding with clots and a lot of pain. So with this in mind, I’ve sadly had to cancel my @LuckyThingsBlog night out tomorrow evening in aid of stayed rested. I just can’t run any additional risk of infection at this point.

So here we are today, Friday 6th – 2 days post operation. I feel ok in myself, still. I woke several times in the night with bad cramps – but after a few painkillers and a bit of To Kill A Mockingbird, I could cope and go back off to sleep. I feel generally achy (hips & back, must be from the procedure positioning) and my pretty bruised – I also have a massive ulcer in my mouth, from where the breathing tube went down my throat.
I have moments of sadness and waves of positivity. I’m mostly sleeping. Not really got a major appetite – though, as usual, I can drink my weight in water. So that’s fine. I’m not allowed to have a bath / stay in the shower for too long (again, risking infection due to open cervix) and I’ve got to keep those dashing surgical stockings pulled up to my knee’s (which is also fine, considering the cold snap – I have pleasantly toasty legs!).
I’ve been sent the most amazing Get Well flowers, plants, cards & chocolate. But mostly? I’m overwhelmed by the kindness I’ve seen in messages and comments – from friends and strangers alike. I appreciate every single one.
This has, so far, been my Miscarriage journey. Whilst I wouldn’t wish this experience on even my worst enemy, I do hope that in sharing my experiences, I have helped someone else. Just one person. This has been a truly cathartic process – and necessary for me. For me to heal and come to terms with things. It’s not for everyone – but if you feel the need to share, then please, please do. Miscarriage is such a common heartbreak that can happen to anyone. 1 in 4 of us – maybe even 1 in 3 of us. But we’re not just statistics – remember that. Sharing your story can make such a difference – not just to others who are going through the same horrendous journey, but also to those charities such as Tommy’s and The Miscarriage Association – that, as I’ve said before, support crucial research into Pregnancy Loss – something that would not be possible without YOUR stories too.
Thank you from the bottom of my heart for all your kindness, guidance, advice, laughs and positivity. I’m not entirely sure what kind of awful position I would be in if I didn’t have the support of my friends and family both offline AND online. It’s meant the world to me – to us, as a family.
As before – it’s good to talk about things. So please do keep getting in touch and sharing your experiences. It’s the only way we’ll learn.
All my love,
C
✖✖✖